The presentation of the 2022 Annual Report on Maternal Health at the Princess Christian Maternity Hospital (PCMH) in Freetown, Sierra Leone, confirms the need to be there to train human resources, improve mortality surveillance, quality of services and availability of life-saving drugs and supplies, including blood banks. A commitment that continues despite increasing difficulties.
Sierra Leone is one of the countries with the highest maternal mortality rate in the world, exacerbated in recent years by rising food and transport costs, and the consequent difficulty in accessing services. The scarcity of health tools and materials such as gloves and suture thread has further complicated the guarantee of services and the ability to perform even the most essential procedures such as caesarean sections.
“I have been working in cooperation for 12 years, almost always in conflict zones. This in Freetown is the first time in a hospital context, in direct contact with the beneficiary and with the ‘resolution’ of cases,’ – says Claudia Mocci, Cuamm project manager in Freetown -. At the PCMH, the hospital in Freetown that CUAMM has been supporting since 2016, you touch on the need to be there and to stay: if we abandon or if we do not put the utmost attention on the work we do, we risk increasing the already enormous problems that exist. This awareness certainly animates the work of the team: we share day by day criticalities and difficulties but also satisfactions’.
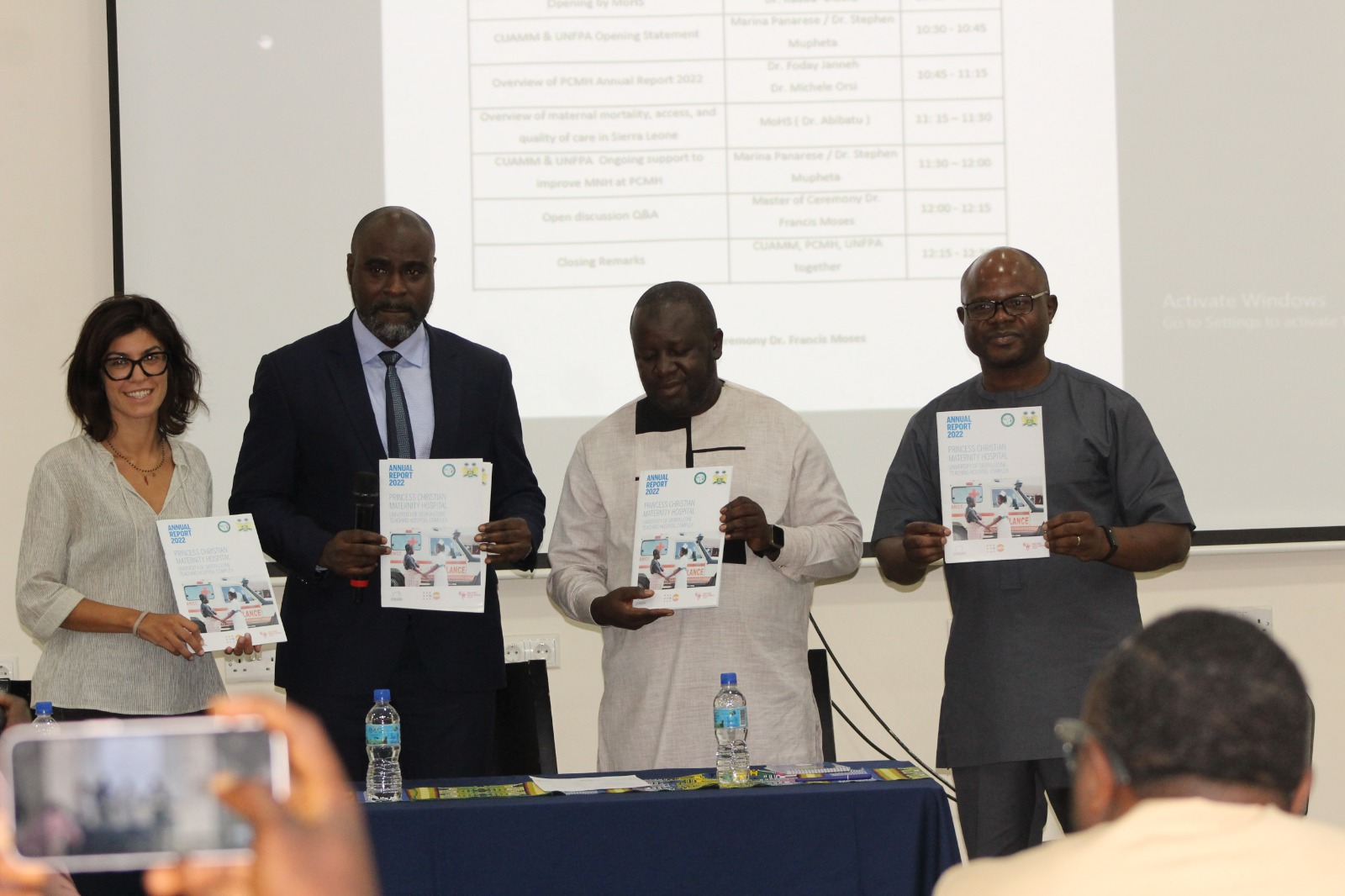
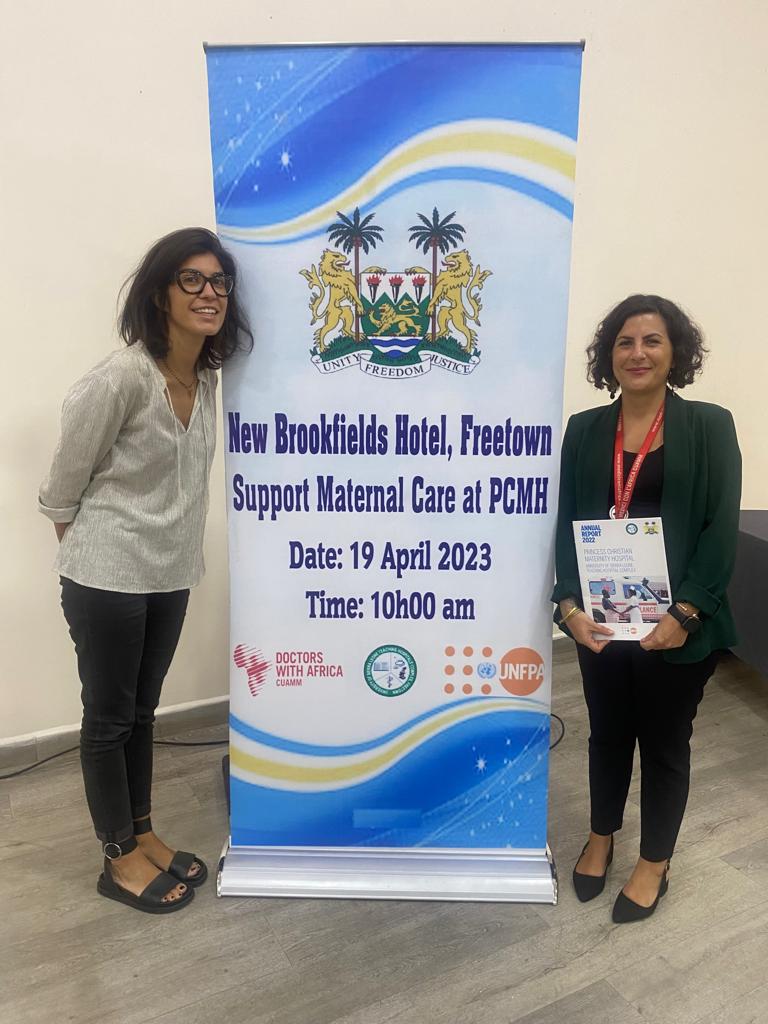 It was in this spirit that the 2022 Annual Report on Maternal Health was presented at the PCMH on Wednesday 19 April. The event was well attended, about 70 people including the hospital’s Medical Superintendent, representatives of the main ministries, UNFPA partners and other NGOs present in the area.
It was in this spirit that the 2022 Annual Report on Maternal Health was presented at the PCMH on Wednesday 19 April. The event was well attended, about 70 people including the hospital’s Medical Superintendent, representatives of the main ministries, UNFPA partners and other NGOs present in the area.
“The collaboration with CUAMM in support of the Ministry has become increasingly solid and fundamental over the years,” said Dr. Mustapha S. Kabba, Deputy Medical Director and representative of the Ministry of Health. The partners must not take the place of the political and governmental actors, who must operate responsibly and fairly, always attentive to the needs of patients’.
At the outset, an overview was given on maternal mortality, access and quality of care in Sierra Leone from 2016 to 2020 with a particular focus on approaches, the heart of the government’s strategic planning, to address the issue.
In line with the ministerial approach, CUAMM presented the good results achieved in support of maternal and child care at the PCMH, with a particular focus on the High Dependency Unit (HDU), the country’s first intensive care unit, launched in 2017 to ensure assistance in the management of the most critical obstetric cases. 337 the total number of admissions in 2022, with a mortality rate of 10.1%, 34 cases, and a referral rate of 5.3% (18 cases). The establishment of HDUs is one of the five pillars of the government’s strategic planning, along with the need for human resource training (postgraduate training, midwifery training, mentoring) and support for specific areas: maternal mortality surveillance for the timely identification and reporting of deaths, review of cases and implementation of measures to prevent similar deaths in the future; improving the quality of services and the availability of life-saving drugs and supplies, including blood banks. These areas, as well as support to the HDU, are at the heart of the current project with the support of the Italian Agency for Development Cooperation and UNFPA.
Despite an improvement in outcomes at the PCMH in recent years, in particular a reduction in maternal and perinatal mortality, efforts must continue and be further consolidated with Sierra Leone to ensure essential, quality care for mothers and babies.