“I used to be scared and sad, not knowing how to handle my emotions, how to share what was happening to me and my thoughts. Then, when we shared in the group what we were going through, I realized I was not alone, and someone was going through and experiencing the same things. I felt listened to, understood.” The sharing of experiences, emotions, and feelings is evident from the words of the young individuals involved in the three-year project “Knowing to Cure” implemented in Beira, Mozambique, by CUAMM and the University of Padua with the support of the Italian Agency for Development Cooperation.
The intervention started in 2021 with the main goal of assessing the impact of Covid-19 on young people with HIV aged between 18 and 24. A seroprevalence study was conducted at 7 Saaj, youth clinics, monitoring access to services before, during, and after the pandemic through six indicators: the number of outpatient visits, HIV tests performed, and HIV positivity rate, the percentage of people not adhering to antiretroviral therapy, the percentage of recall calls (buscas), and return to treatment. Despite an initial decline, the number of outpatient visits and HIV tests in the post-pandemic period showed a trend comparable to that before the pandemic, with an average of 1,487 visits and 419 HIV tests per month. Moreover, even during the emergency, phone calls and home visits proved effective in bringing back to treatment 79.2% of patients who had abandoned it.
Within the project, in addition to supporting and strengthening HIV prevention and treatment activities, dedicated mental health services were activated to address psychological distress related to HIV status as well as more general conditions. 315 adolescents and young people aged 15 to 24, both HIV+ and HIV-, were divided into 30 groups and engaged in weekly awareness sessions on mental health, particularly using psychodrama techniques, to share their thoughts and experiences, enhance awareness, and socio-emotional skills to promote mental and psychological well-being and reduce stigma.

“It was an experience of great responsibility and complexity but also very stimulating and rewarding, especially seeing the impact of services on the community, operators, and the involved youth,” adds Roberto. “Despite the difficulties, I always perceived a great strength and willingness to get involved in changing their own condition.” An extra motivation to continue commitment in this area alongside the communities. Because there is no health without mental health.
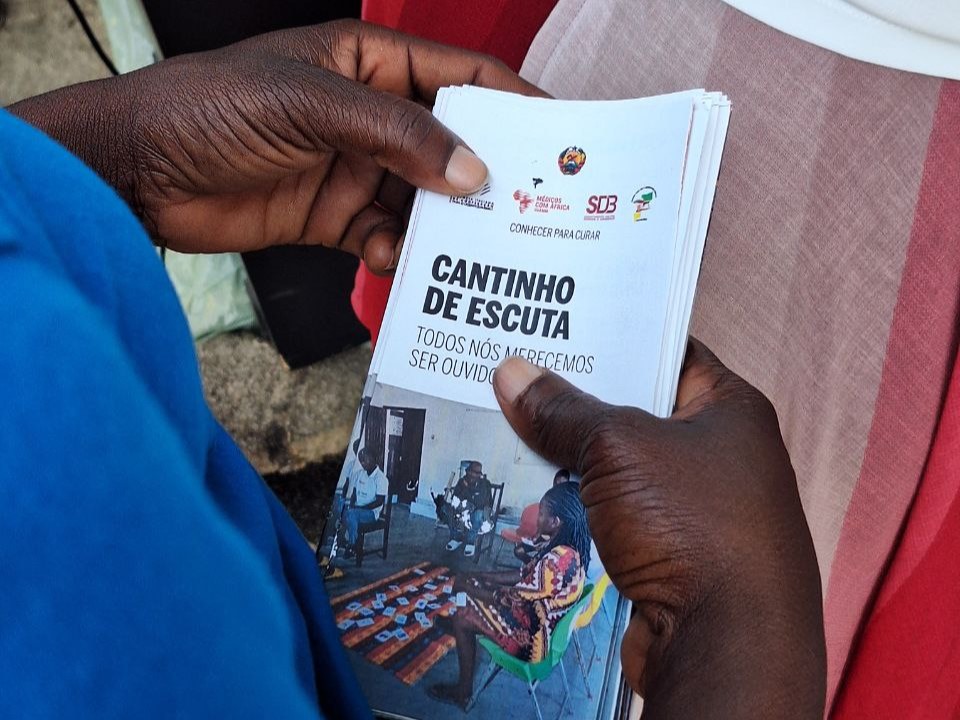
“Listening Corners”: the value of mental health
“We are not used to listening either to others or to ourselves. Sometimes people judge us without realizing the cause behind our behavior. I have learned that it is important to be attentive to others. One cannot help without listening,” said a young participant in the group.
“Even just having had a space and an opportunity to tell my own story was transformative in itself. Feeling to have a voice, value, recognizing oneself in the words and experiences of others created a strong connection among them,” explains Chiara Malesani, a neuropsychiatrist who followed the activities with the youth.
From this space of sharing and confrontation, incredible experiences emerged, stories of distress and vulnerability that made the need to increase awareness regarding mental health even more evident, sensitizing on the importance of taking care of one’s inner and emotional self and promoting support services. “This part of the intervention was really challenging, especially because it is a little-known and discussed topic in that context,” says Roberto Benoni, project leader in Beira. “I remember that during the focus groups with the kids, vignettes were used to illustrate various issues such as domestic and gender-based violence and suicide.”
According to 2019 data from the World Health Organization, Mozambique has one of the highest suicide rates in Africa and the world, at 13.6 per 100,000 people. Not numbers but individuals expressing a need to which this intervention sought to provide a first response.
At the health facilities, psychology services were strengthened by introducing a registry to improve patient data collection and provide a clinical monitoring tool, ensuring follow-up visits. In particular, in two psychology services, four community health workers were trained to sensitize the community on mental health and make reminder calls (lembrete) to increase adherence to psychology consultations.
A part of the intervention was dedicated to the establishment and management of cantinhos de escuta, “listening corners” freely accessible places located in strategic points (markets, neighborhood offices, etc.) where people in need could go to talk about their psychological and social problems, finding empathetic and active listening activists on the other side. “I was glad to know that local authorities decided to continue the service of listening corners, recognizing the value and utility that this service has for the community,” says Roberto. At the listening corners, a mental health screening activity took place, and those who tested positive were directed to health facilities and recalled after 15 days to check if they had attended the visit. Between September and December 2023, 458 people underwent screening, and 174, 38%, tested positive. Among the positives, 94 did not attend the visits, citing reasons such as fear of judgment, lack of time, and the impossibility of finding a nearby psychologist. This shows that there is still much work to be done to combat stigma and raise awareness of the importance of self-care.