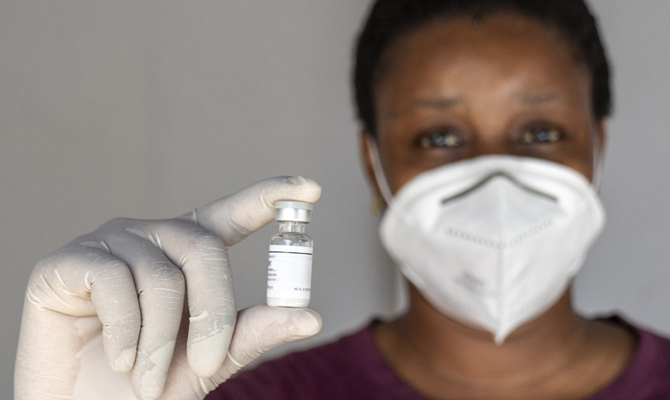
Monday Jan 22, the first malaria immunization campaign started in Soa, a village 20 km away from the capital Yoaundé under the supervision of WHO, GAVI and UNICEF. Cameroon is the first country to roll out the immunization campaign following successful trials in Ghana, Kenya and Malawi. The RTS,S vaccine also known as Mosquirix, will be administered in 42 districts and 10 counties across the country both in health centres and private clinics. The rollout started after the delivery of about 331.120 jabs in November 2023.
PILOT PROGRAM
Since 2019, Ghana, Kenya, and Malawi have been administering the vaccine in a schedule of 4 doses from around 5 months of age in selected districts as part of the pilot program, known as the Malaria Vaccine Implementation Programme (MVIP). 2 million children received the immunization. According to WHO, the first malaria vaccine has contributed to reduce child deaths by 13% in 4 years. The results also demonstrated that severe malaria was reduced by 22% in children who received 3 doses, reduction was also recored in hospitalization. Other African countries have already planned to introduce the vaccine this year, with hopes that 6.6 million children could be reached. Deliveries are due for Burkina Faso, Liberia, Niger and Sierra Leone.
«There are numerous challenges ahead – says Giovanni Putoto, Head of Planning and Operational Research at CUAMM, since, as we all know, Africa does not only struggle to access vaccines. Once again, the major challenges is to transform vaccine into immunization, that is what we have experienced in the past years during the Covid-19 pandemic. In order to do so, cross efforts from both governments and international partners are essential. The major challenges we will be call to address? Of course vaccine shipment and storage but also vaccine skepticism and false information, insufficient knowledge of the malaria vaccine among health workers and last but not least, inadequate funding and resource allocation needed to ensure the administration of the 4 doses. These are all aspects concerning the functioning of the health system».
About a week after the campaign’s kick-off concerns about low participation in the immunization campaign have already risen showing the consequences of little knowledge of the vaccine’s benefits among both communities and health workers. At the same time, while WHO together with the scientific community warn the public to integrate preventive tools such as bed nets and chemoprophylaxis with vaccine administration, research continues on a second vaccine: R21. The WHO has recommended R21 for the prevention of malaria in children in October 2023. Although both vaccines are shown to be safe and effective in preventing malaria in children, available supply of RTS,S is limited. The addition of R21 is therefore expected to result in sufficient vaccine supply to benefit all children living in areas where malaria is a public health risk. Moreover, the cost-effectiveness of the R21 vaccine would be higher than RTS,S which cost per dose administered is now estimated around US$10 against US$ 2 – 4 due for R21. Results from the clinical trials have demonstrated the latter’s high efficacy especially when administered before the rainy season.
MALARIA IN AFRICA
Malaria remains a major cause of disease and mortality worldwide. Plasmodium falciparum, which is the cause, is a parasite that is transmitted to humans by infected female mosquitoes belonging to the genus Anopheles.
«The vaccine that was studied, recommended and that is now being administered is revolutionary because it fights a pathogen as complex as the malaria parasite, which is constantly changing and able to escape our immune system», stated Giovanni Putoto.
In 2022 alone, 186,318,000 malaria cases have been recorded across 12 major African markets namely: Burkina Faso, Cameroon, DRC, Ghana, Kenya, Mali, Mozambique, Niger, Nigeria, South Africa, Tanzania and Uganda. According to scientists, this datais expected to rise to 211,098,000 by 2027.
According to WHO, in 2021 alone 619,000 death accurred worldwide due to malaria and 247,000 cases were diagnosed globally with Africa carrying the burden of 95% of cases. Africa also counts for 80% of malaria deaths in children under 5 years of age.
Doctors with Africa CUAMM works in 8 African countries where it keeps up its committment to scale up malaria prevention, diagnosis and treatment starting from the hardest-to-rich villages to communities, to health centres, up to the main hospitals. In 2022 alone, CUAMM registered 1,666,785 cases of malaria treated, including 744,182 children under the age of 5 in 6 of the 8 countries in which it operates namely: Ethiopia, Central Africa, Mozambique, Sierra Leone, South Sudan, Tanzania and Uganda.