Less than a century ago, the fortunate discovery of penicillin revolutionized medicine: until 1929, the world had to contend with daily deaths caused by infections without effective treatments. Today, however, millions of lives are at risk due to infections that no longer respond to available therapies: this is the threat of antimicrobial resistance. To raise awareness about this issue, the WHO has been observing the World Antimicrobial Awareness Week every year since 2015, from November 18 to 24.
A Global Health Threat
Numerous studies have highlighted that the danger now lies not only in pathogens themselves but also in the mechanisms these microorganisms adopt to defend against our attacks. This phenomenon, known as antimicrobial resistance (AMR), represents a global health emergency. Bacteria, viruses, fungi, and parasites can develop mechanisms that make them resistant to drugs designed to kill them or inhibit their growth—these drugs being antimicrobials.
Within this broader issue, the international community is particularly concerned about antibiotic resistance: the ability of bacteria to resist the action of antibiotics and pass this adaptation on to future generations. This undermines the effectiveness of standard treatments, severely impacts healthcare quality, and turns even common infections into potentially fatal conditions. The rise of antibiotic resistance is driven by the overuse of antibiotics in humans and in hospital settings. However, it is also closely linked to environmental factors, such as the use of antibiotics in livestock and agriculture and poor hygiene and sanitation systems with improper disposal of wastewater containing partially active antibiotics.
Antibiotic Resistance: A Serious and Growing Global Concern
WHO estimates reveal the severity of the phenomenon: antibiotic resistance is already a significant cause of mortality. Globally, it is estimated that 1.27 million deaths per year (WHO) are due to antibiotic-resistant infections. In the African region alone, around 250,000 deaths annually are directly attributable to antibiotic-resistant bacteria.
The African Continent
In resource-limited settings where infectious, sexually transmitted, and tropical diseases have high incidence rates, antibiotic resistance takes on even greater significance. Africa accounts for 95% of global malaria deaths, 70% of people living with HIV, and 25% of tuberculosis-related deaths (Africa CDC). In 2019 alone, antibiotic resistance was linked to 55,000 deaths from HIV and 30,000 deaths from malaria, underscoring the severity of the crisis in the region. Beyond the misuse and overuse of antimicrobials, additional factors exacerbate the impact in African nations: migration, low vaccination rates, environmental contamination from pharmaceutical and hospital waste, lack of access to clean water and sanitation, inadequate infection prevention measures, and limited knowledge and training. Antimicrobial resistance places additional strain on health systems, as standard treatments become ineffective, hospital stays lengthen, and healthcare costs rise.

CUAMM’s Operational Research on the topic
Antibiotic resistance is a complex and interdisciplinary issue that spans clinical care, epidemiological surveillance, and public health. This holistic perspective has shaped CUAMM’s collaborative research efforts to deepen field knowledge in Uganda.
The Opt-AMR project, led by the Centre for Infectious Disease Control in Zambia (CIDRZ) and involving the Makerere University (Uganda), Malawi-Liverpool Wellcome Trust Centre (MLW), Medici con l’Africa CUAMM, and Liverpool School of Tropical Medicine, focuses on investigating fever management and antibiotic administration in children. The study addresses both the biological dimension of antibiotic resistance—collecting samples to directly examine bacterial populations—and the community dimension, analyzing how care is managed and treatments are administered. In resource-limited settings, healthcare workers, community health providers, traditional healers, and medicine vendors are often the first responders in treating childhood febrile illnesses, offering support to mothers. Understanding the processes of diagnosis, care management, and antibiotic administration is essential to identifying whether and how unnecessary broad-spectrum antibiotics are being used, and how interventions can improve these practices.
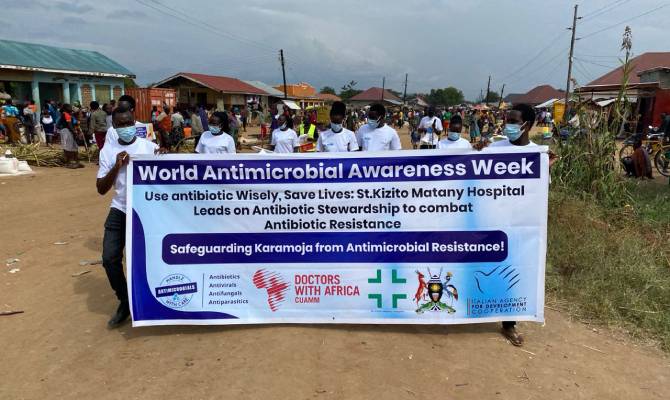
Another research initiative, Advancing Antibiotic Resistance Surveillance and Harnessing Antimicrobial Stewardship in the Karamoja Sub-region (ARSK), linked to the ALL IN ONE project in Uganda’s Karamoja region, explores antibiotic use patterns and the knowledge, attitudes, and prescribing practices of healthcare professionals at St. Kizito and Moroto hospitals. These insights will inform updates to clinical guidelines for antibiotic prescribing, hygiene practices, and patient education. Collaborating with Makerere University and the Uganda National Council for Science and Technology, the research also examines samples from hospital surfaces (e.g., floors, workstations) as well as from healthcare workers and the general population to study bacterial population responses to antibiotic use.
Strengthening Global Partnerships
CUAMM’s operational research has recently expanded to include collaboration with the World Health Organization as part of the Infection Prevention and Control (IPC) network. By rigorously analyzing hospital practices to minimize infection risks, identifying gaps, and implementing improvement strategies, CUAMM aims to limit the emergence of resistant bacteria and safeguard public health.
A Global “One Health” Approach
Antimicrobial resistance (AMR) is a challenge that transcends medicine, connecting human, environmental, and animal health within the One Health framework. Addressing this crisis requires integrated actions, including research, training, prevention, and policy development, to mitigate the impact of a growing threat to public health worldwide.
CUAMM’s work in the field
In Uganda, CUAMM works to prevent and respond to the outbreak of zoonotic diseases in the northern region of Karamoja thanks to All in One project, implemented in collaboration with Africa Mission and with the financial support of the Italian Cooperation Agency for Cooperation and Development (AICS).