CONTEXT
The Central African Republic (CAR) has a population of 4.8 million. It is one of the poorest and most fragile countries in the world despite its wealth of natural resources. CAR has been suffering chronic instability since its independence in 1960: the cycle of violence does not seem to stop as the recent clashes between the national armed forces and armed groups show, forcing thousands of people to flee. Indeed, more than 630,000 people remain internally displaced while as many people are refugees in neighbouring countries (UNHCR data). The Central African Republic still ranks among the worst-off countries in the Human Development Index (188th out of 189), with more than half of the population in need of humanitarian assistance. The health indicators are also really poor:
- Infant mortality rate: 84.5 per 1,000 live births
- Under-five mortality rate: 116.5 per 1,000 live births
- Maternal mortality rate: 829 per 100,000 live births
CAR health system suffers from ineffective financing, insufficient supply of medicines, limited coverage and uptake of essential health services, further worsened by the Covid-19 pandemic. About 70 per cent of health services are provided by humanitarian organizations.
THE PROJECT “APPUI AU COMPLEXE HOSPITALIER UNIVERSITAIRE PÉDIATRIQUE DE BANGUI”
The health programme of the Bêkou Fund (Santé II), funded by the European Union, aims to strengthen health service delivery, governance and leadership in the health care sector. The goal of Santé II is to support the health system in the transition between the crisis (Santé I programme, which run from 2013 to 2015) and the development phase (Santé III programme, running from 2019 to 2021).
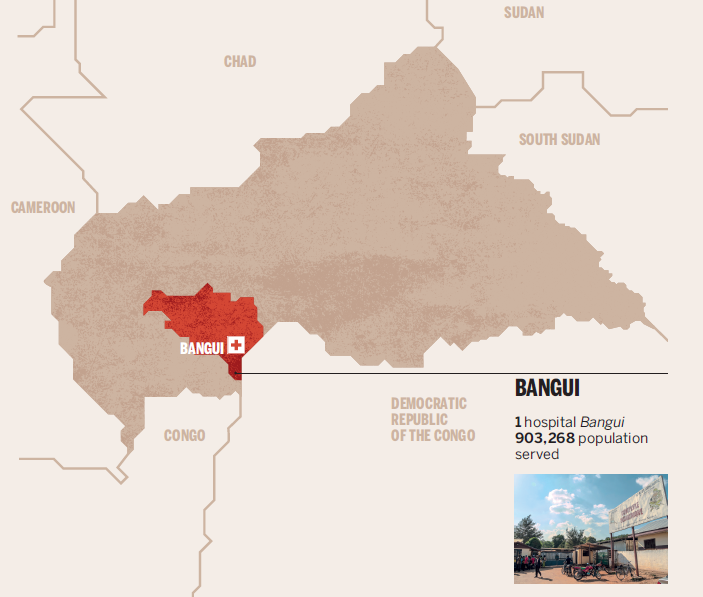
Within this framework, the Bêkou Fund of the European Commission financed the project “Appui au Complexe Hospitalier Universitaire Pédiatrique de Bangui” (Support to Bangui Paediatric Hospital) to contribute to improve the health status of vulnerable groups, such as children, by ensuring access to quality health care at Bangui Paediatric Hospital, through capacity building of the hospital management team and health staff.
Bangui Paediatric University Hospital (Complexe Hospitalier Universitaire Pédiatrique de Bangui, CHUPB) is the only paediatric hospital of the country. It is the referral hospital for specialist paediatric care, including integrated treatment of severe acute malnutrition and paediatric surgery. It is also a training centre for all human resources for health in the country. It therefore has a crucial role for the health of children in CAR.
Doctors with Africa CUAMM and the French NGO Action contre la Faim (ACF) are working together to implement this project, which has been running since the 1st of July 2018. The expected results of the intervention are the continuous provision of quality free health-care for general paediatric patients and patients affected by SAM (Severe Acute Malnutrition), and a strengthened training system for current and future human resources for health at the hospital.
In order to achieve these results, the project implements a strategy of technical assistance and mentorship to both management staff and clinical staff, aimed at strengthening provision of care, hospital administration, human resources management, and procurement and management of medicines. By doing so, the objective is also to strengthen the overall management of the hospital and the health information system. This will improve the monitoring and evaluation system of hospital indicators and thus support the hospital in planning its services based on objective data. This contributes therefore to the creation of a more favourable environment for the training of medical and paramedical students and hospital staff (including through internships).

KEY ACHIEVEMENTS (July 2018–May 2021)
202,593 children had access to the triage of the hospital
55,380 children had been admitted, in particular
- 5,202 in Intensive Care Unit
- 4,005 in Neonatology
- 34,695 in the Medical Units A, B, C
- 6,061 in Inpatients Nutrition Therapeutic Unit
5,333 children were admitted in the surgery department
RESULTS ACHIEVED SO FAR
Governance: The governance structures of the hospital were reactivated (medical and clinical meetings, administrative and financial committee meetings, and the Comité de Gestion (Management meeting). The governance capacity of the hospital has improved, as demonstrated also by the elaboration of its first Annual Report in 2018 and 2019.
Financing: The administrative capacities of the hospital have been analysed through needs’ assessment missions and a costing exercise to determine the costs of the malnutrition unit. An action plan was designed to improve Hospital’s accountancy and Human Resources’ management systems.
Infrastructure: the project supported the organisational revision of some services (Nutrition unit, Triage, and Emergency services).
Health Workforce: A motivational bonus has been set up to integrate the staff’ monthly salary. Staff members were trained on various themes in paediatric care (including nutritional rehabilitation).
Information, Analysis and data-driven research: The Statistics office was strengthened in terms of IT material, skills and capacities. The Hospital Health Management Information System (HMIS) record was reviewed thoroughly, as well as the diagnosis system in use in light of WHO international classification of diseases. New formats for medical records for all the departments of the hospital have been elaborated. Data-driven analysis and evaluation was conducted on paediatric and newborn health, and the results presented by hospital’s staff in national fora.
Supply chain & health inputs: continuous maintenance of biomedical devices, fans, generators, cars, computer equipment, electrical, hydraulic and sewer systems hes been guaranteed. In the pharmacy, an opensource management software was introduced to improve planning, distribution, and storage of medicine supply. A handbook of pharmaceutical procedures was developed to ensure written and codified procedure.
Service quality: quality health care has been provided for free, 24/7. A team made by the hospital’s paediatricians, the hospital’s Direction and Cuamm’s technical assistants reviewed and updated the Hospital’s paediatric and neonatal clinical guidelines and protocols. The hospital’s Inpatient Nutrition Therapeutic Unit is the only structure providing free Integrated Management of Acute Malnutrition for under-five children, 24/7.
COPING WITH COVID-19
The arrival and spread of Covid-19 in the Central African Republic, with the first case reported on 14 March 2020, has put a strain on the already limited capacities of the national health system. In light of this, the CAR Ministry of Health and Population (MSP) and the World Health Organisation (WHO) invited partners to engage in the implementation of the action plan for emergency preparedness and response to Covid-19.
Therefore, it has been necessary for the health personnel to gain knowledge, information and skills on Infection and Control (ICP). The same applied for patients and their care takers who needed to be made aware of the issue, and how to prevent it. Raising- awareness activities have been fundamental to overcome rumours and misperceptions about Covid-19, demystifying this epidemic.
A set of actions have been implemented to face the pandemic:
- Information and Awareness, particularly on routes of transmission, prevention measures, correct hygiene practices, social distancing etc., through reproduction and display of brochures and posters in French and in Sango, focus groups discussion, among others;
- Communication: regular radio broadcasts (French and Sango) on the rules of access and conduct at the CHUPB, screening and distancing.
- Hygiene And Environment: setting up of several points for hand washing and disinfection with chlorinated water containers and the provision of soap, including home-made production of hydro-alcoholic solution, visors, and masks.
- Training of all hospital staff so that they can learn the proper procedures related to Covid-19, and for the use of personal protective equipment;
- Management: establishment of a Medical Committee to cope with the pandemic, such as restrictions on visits, the respect of distancing, the establishment of an external route to the Units dedicated to all suspicious cases, sensitisation of all accompanying persons about Covid-19 and the measures to be followed in the hospital; the establishment of a “red zone” hospitalization.
- Supply of essential drugs, consumables, laboratory materials, and personal protective equipment, considering however the extreme difficulty to find them and importing into the country.
All daily activities have been therefore adapted to the new challenging circumstances, trying to ensure the continuity of the essential healthcare and raising community awareness on the issue in order to guarantee the access and use of services, along with good health and nutrtion practices.

https://ec.europa.eu/europeaid/bekou-trust-fund-introduction_en
This publication was produced with the financial support of the European Union. The contents are the sole responsibility of Doctors with Africa CUAMM and do not necessarily reflect the vision of the European Union.